Galeria
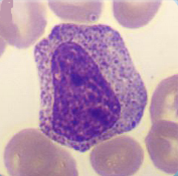
In this maturation stage the separation into the 3 different subpopulations of granulocytes occurs by development of specific granulation for each (secondary granulation).
Cell description:
Size: 10-18 µm
Nucleus: oval or slightly indented with variable degree of chromatin clumping, nucleoli usually not apparent
Cytoplasm: acidophilic neutrophil: primary azurophilic and secondary neutrophilic granules
<p>In this maturation stage the separation into the 3 different subpopulations of granulocytes occurs by development of specific granulation for each (secondary granulation). </p> <p>Cell description: </p> <p>Size: 10-18 µm </p> <p>Nucleus: oval or slightly indented with variable degree of chromatin clumping, nucleoli usually not apparent </p> <p>Cytoplasm: acidophilic neutrophil: primary azurophilic and secondary neutrophilic granules</p>
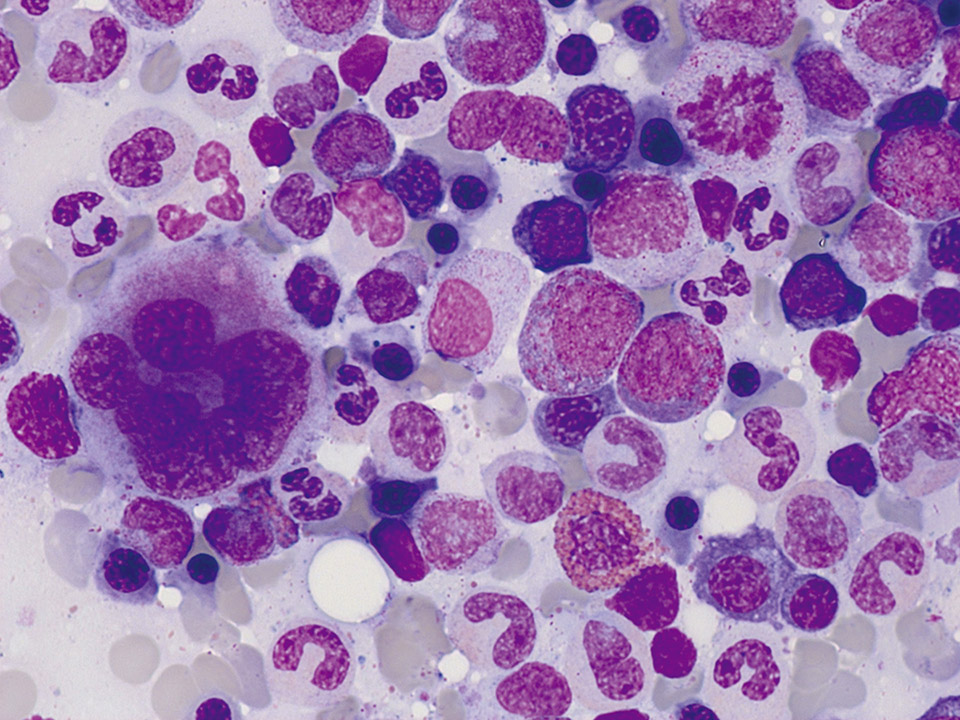
Normal bone marrow cytology. Some cells are always squeezed and damaged. These cells are called smudge cells. Smudge cells cannot be examined and must not be regarded as pathological (They have nothing to do with Gumprecht shadows in the peripheral blood smear). On the top right a mitosis is visible.
<p>Normal bone marrow cytology. Some cells are always squeezed and damaged. These cells are called smudge cells. Smudge cells cannot be examined and must not be regarded as pathological (They have nothing to do with Gumprecht shadows in the peripheral blood smear). On the top right a mitosis is visible. </p>
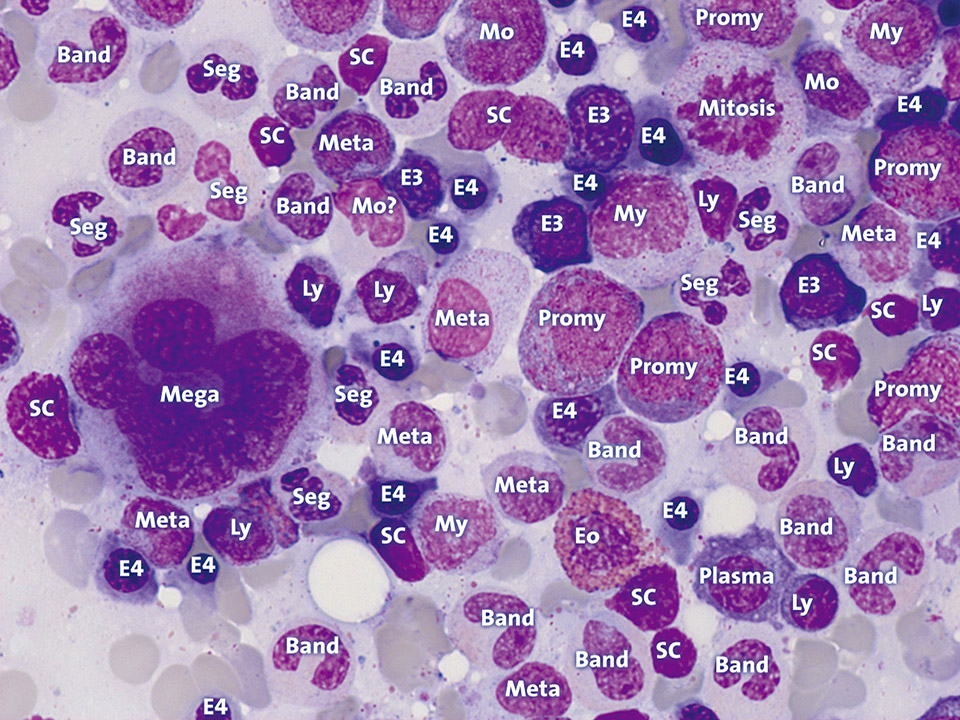
The abbreviations mean: Band: Band neutrophil, E3: Polychromatic erythroblast, E4: Orthochromatic erythroblast, Eo: Eosinophil granulocyte, Ly: Lymphocyte, Mega: Megakaryocyte, Meta: Metamyelocyte, Mo: Monocyte, My: Myelocyte, Plasma: Plasma cell, Promy: Promyelocyte, SC: Smudge cell, Seg: Segmented neutrophil, ?: No clear assignment possible.
<p>The abbreviations mean: Band: Band neutrophil, E3: Polychromatic erythroblast, E4: Orthochromatic erythroblast, Eo: Eosinophil granulocyte, Ly: Lymphocyte, Mega: Megakaryocyte, Meta: Metamyelocyte, Mo: Monocyte, My: Myelocyte, Plasma: Plasma cell, Promy: Promyelocyte, SC: Smudge cell, Seg: Segmented neutrophil, ?: No clear assignment possible.</p>
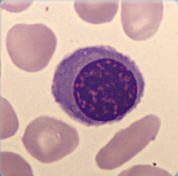
Cell description: 3 different stages of nucleated red blood cells are known: basophilic, polychromatic and orthochromatic
Size: around 10 µm
Nucleus: round with variable degree of chromatin condensation according to maturation, faint or absent nucleoli
Cytoplasm: bluish to pink (depending on maturation), no granules
Nucleus decreases in size as the cell matures
<p>Cell description: 3 different stages of nucleated red blood cells are known: basophilic, polychromatic and orthochromatic </p> <p>Size: around 10 µm </p> <p>Nucleus: round with variable degree of chromatin condensation according to maturation, faint or absent nucleoli </p> <p>Cytoplasm: bluish to pink (depending on maturation), no granules </p> <p>Nucleus decreases in size as the cell matures</p>
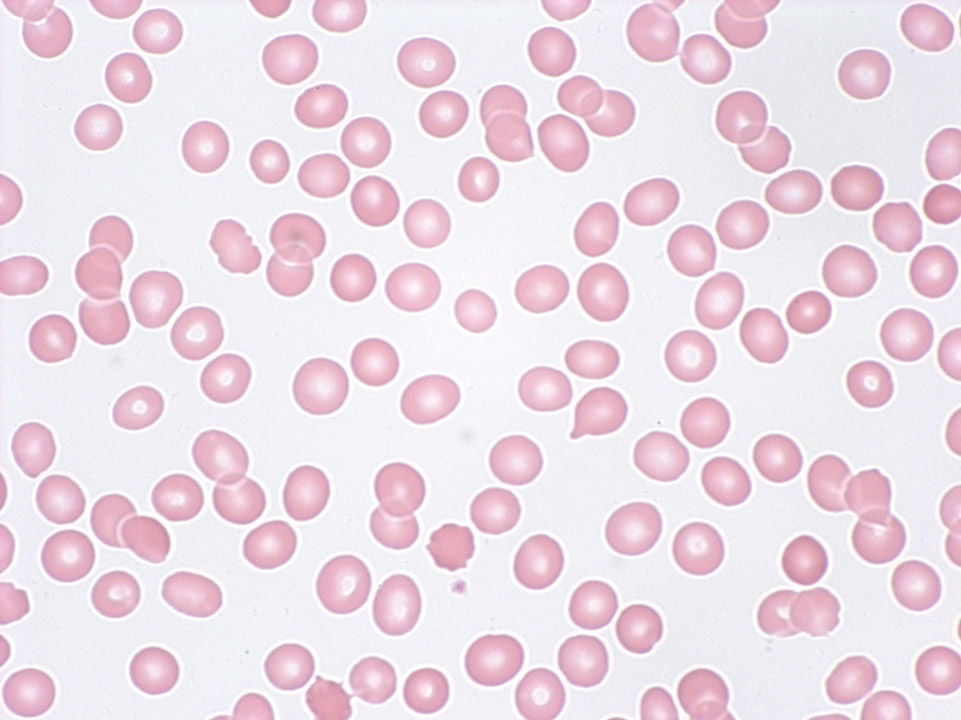
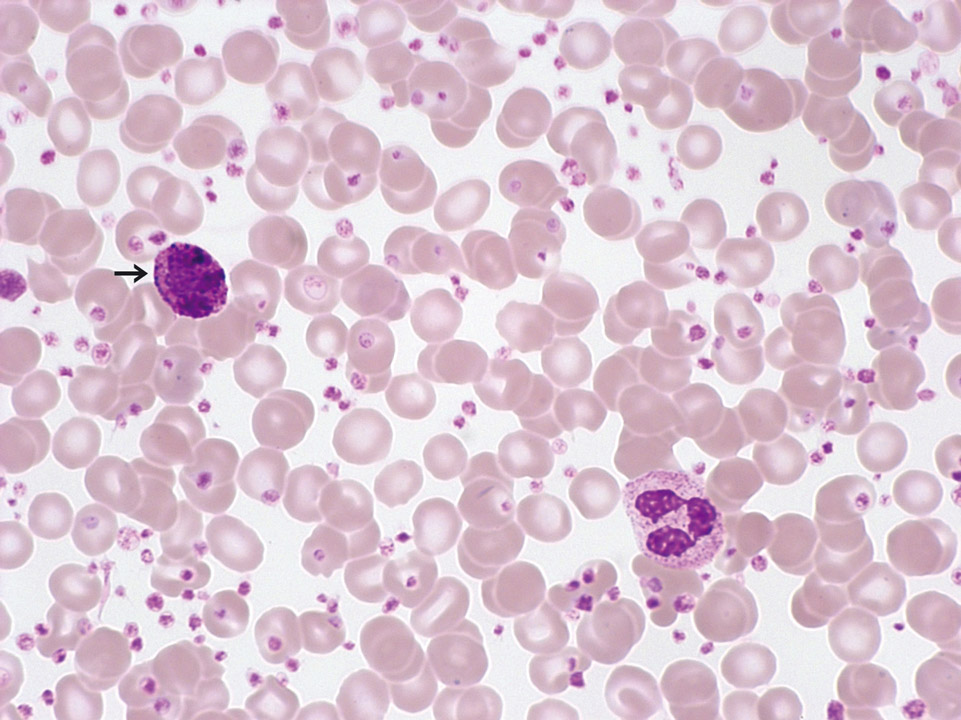
Pancytopenia (tricytopenia) in the peripheral blood (May-Grünwald-Giemsa stain) of a patient with severe aplastic anaemia: The automated cell count showed granulocytopenia (300/µL), mild lymphocytopenia (800/µL), anaemia (haemoglobin 9 g/dL), a reduced reticulocyte count (18,000/µL) and thrombocytopenia (12,000/µL).
<p>Pancytopenia (tricytopenia) in the peripheral blood (May-Grünwald-Giemsa stain) of a patient with severe aplastic anaemia: The automated cell count showed granulocytopenia (300/µL), mild lymphocytopenia (800/µL), anaemia (haemoglobin 9 g/dL), a reduced reticulocyte count (18,000/µL) and thrombocytopenia (12,000/µL).</p>
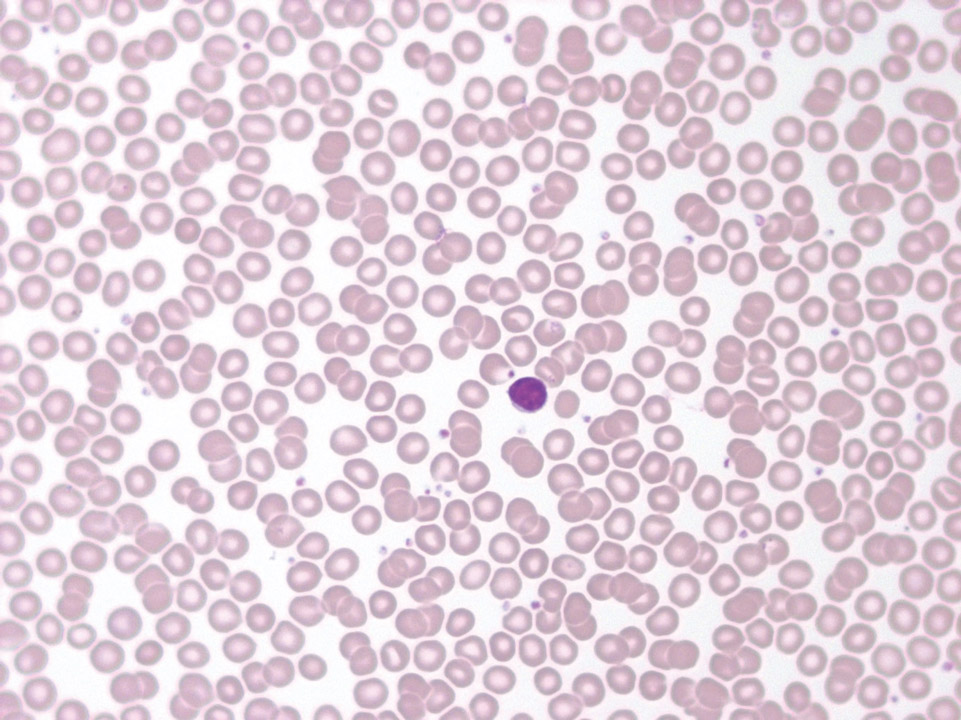
The peripheral blood (May-Grünwald-Giemsa stain) of this patient shows only isolated neutropenia (900/μL) with morphologically normal red blood cells and normal red blood cell and platelet counts. Aplastic anaemia is not present. A lymphocyte can be seen in the middle.
<p>The peripheral blood (May-Grünwald-Giemsa stain) of this patient shows only isolated neutropenia (900/μL) with morphologically normal red blood cells and normal red blood cell and platelet counts. Aplastic anaemia is not present. A lymphocyte can be seen in the middle.</p>
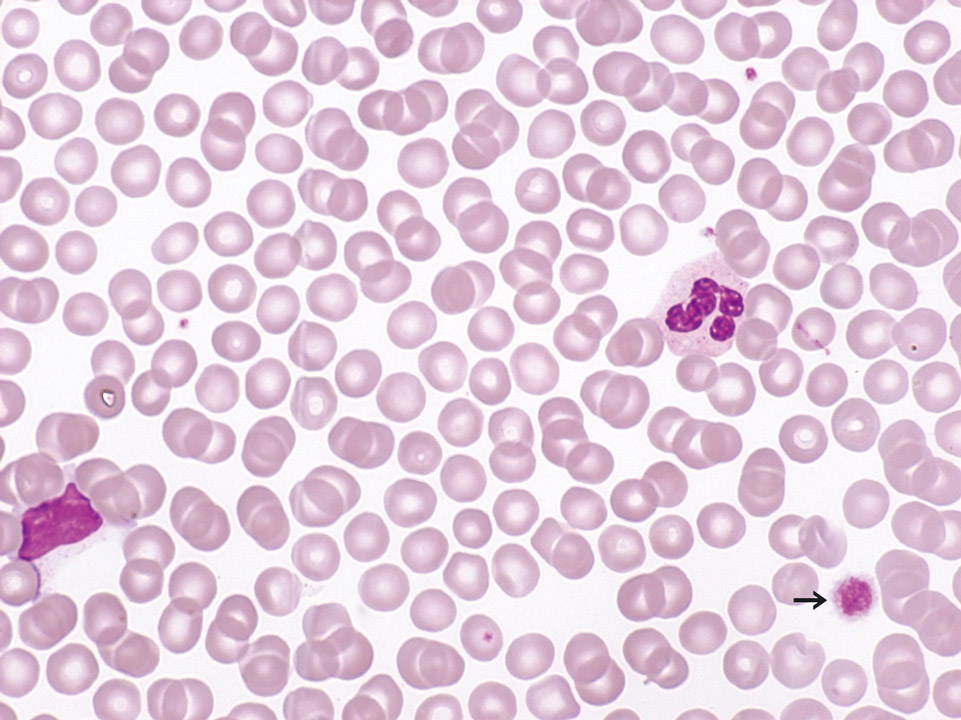
Peripheral blood (May-Grünwald-Giemsa stain) of a patient with B-CLL. The few platelets are mostly large (->) (= platelet anisocytosis). Here a secondary immune thrombocytopenia (ITP) was evoked by immunoglobulin-producing lymphoma cells. The immunoglobulins react with proteins on the platelet surface, leading to an elimination of these platelets from the peripheral blood.
<p>Peripheral blood (May-Grünwald-Giemsa stain) of a patient with B-CLL. The few platelets are mostly large (->) (= platelet anisocytosis). Here a secondary immune thrombocytopenia (ITP) was evoked by immunoglobulin-producing lymphoma cells. The immunoglobulins react with proteins on the platelet surface, leading to an elimination of these platelets from the peripheral blood.</p>
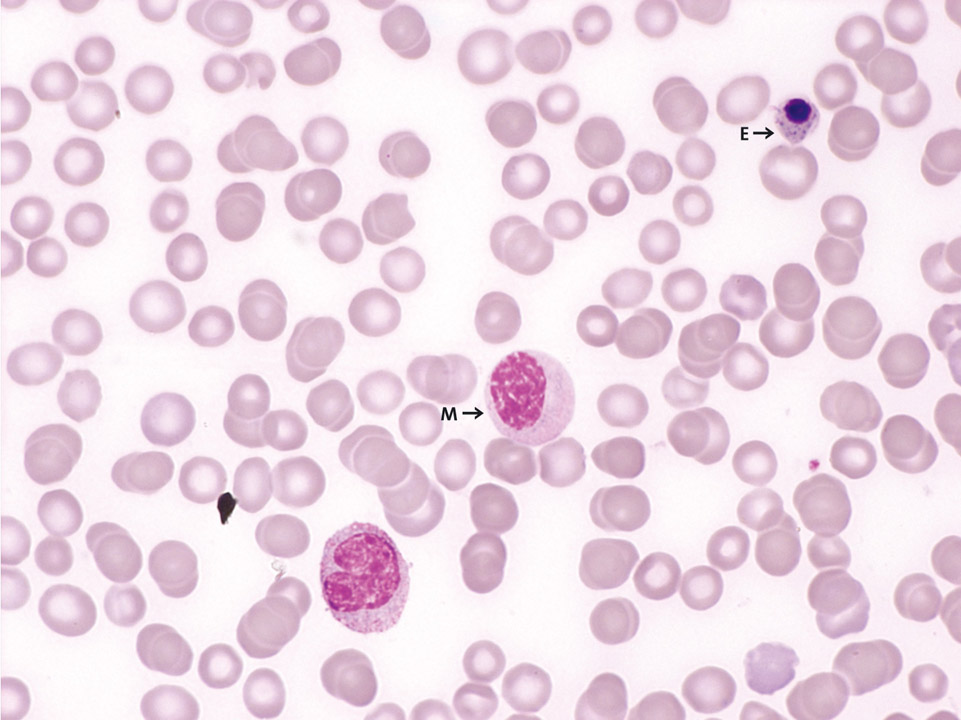
The peripheral blood (May-Grünwald-Giemsa stain) of a patient with breast cancer and bone metastases demonstrates a leucoerythroblastic picture. There are left-shifted granulopoiesis (e.g. here a myelocyte (M)), erythroblasts (E) and distinct thrombocytopenia.
<p>The peripheral blood (May-Grünwald-Giemsa stain) of a patient with breast cancer and bone metastases demonstrates a leucoerythroblastic picture. There are left-shifted granulopoiesis (e.g. here a myelocyte (M)), erythroblasts (E) and distinct thrombocytopenia.</p>
Peripheral blood (May-Grünwald-Giemsa stain) of a 27-year old patient with chronic myelogenous leukaemia (CML). Normal red blood cells, marked thrombocytosis (2,750,000/µL), increased basophilic granulocytes (->) and a normal white blood cell count are observed. In this case no JAK2 mutation could be detected; instead the patient was tested positive for the BCR-ABL fusion gene.
<p>Peripheral blood (May-Grünwald-Giemsa stain) of a 27-year old patient with chronic myelogenous leukaemia (CML). Normal red blood cells, marked thrombocytosis (2,750,000/µL), increased basophilic granulocytes (->) and a normal white blood cell count are observed. In this case no JAK2 mutation could be detected; instead the patient was tested positive for the BCR-ABL fusion gene.</p>