Galeria

Bone marrow histology of a patient with breast cancer showing an infiltration of the bone marrow by a lobular carcinoma of the breast. The increased number of fibres is coloured black after Gomori staining.
<p>Bone marrow histology of a patient with breast cancer showing an infiltration of the bone marrow by a lobular carcinoma of the breast. The increased number of fibres is coloured black after Gomori staining.</p>
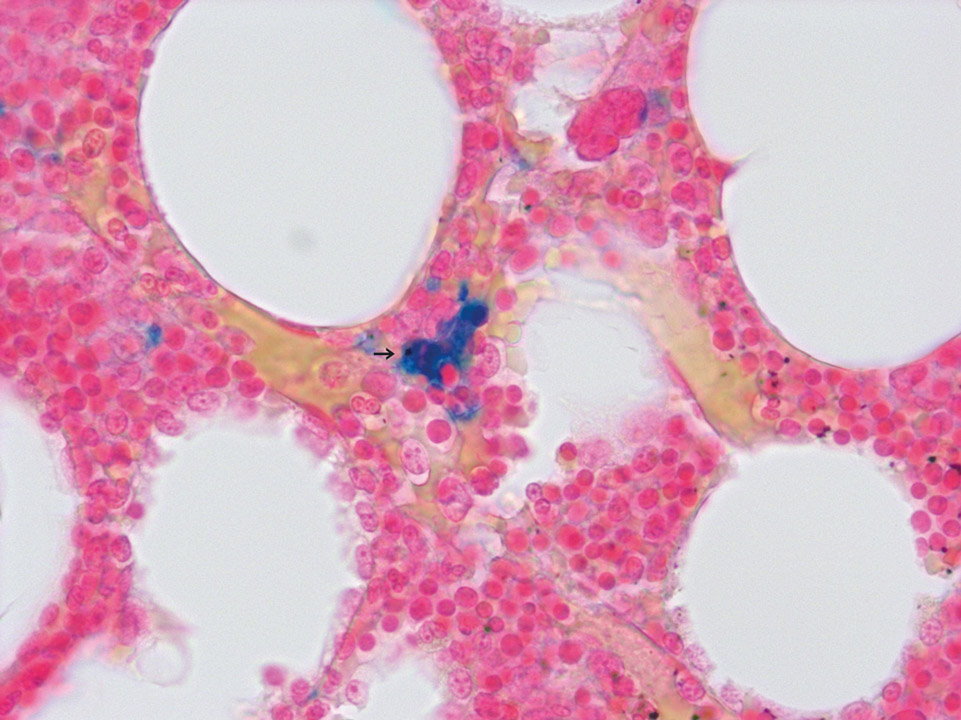
Due to an increased production of red blood cells in PV iron in the bone marrow gets 'used up', causing functional iron deficiency in the bone marrow. The detection of iron accumulation (->) in the bone marrow by Prussian Blue stain, as shown here, argues against PV.
<p>Due to an increased production of red blood cells in PV iron in the bone marrow gets 'used up', causing functional iron deficiency in the bone marrow. The detection of iron accumulation (->) in the bone marrow by Prussian Blue stain, as shown here, argues against PV.</p>
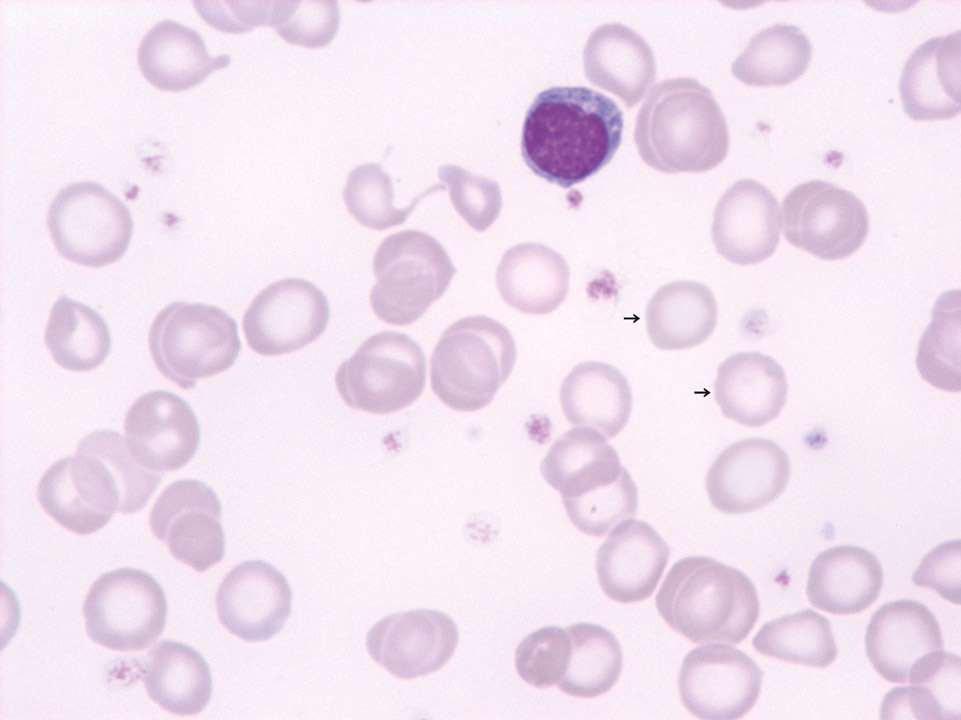
Patient with established severe iron deficiency anaemia (haemoglobin 5 g/dL). Well recognisable are anulocytes (->) and unusually small red blood cells – compared to a normal lymphocyte. The MCV was 53 fL.
<p>Patient with established severe iron deficiency anaemia (haemoglobin 5 g/dL). Well recognisable are anulocytes (->) and unusually small red blood cells – compared to a normal lymphocyte. The MCV was 53 fL.</p>

Peripheral blood (May-Grünwald-Giemsa stain) of a patient with isolated congenital reduction of erythropoiesis in the bone marrow (pure red cell aplasia, PRCA). The haemoglobin concentration was 9.2 g/dL, white blood cell and platelet counts were normal.
<p>Peripheral blood (May-Grünwald-Giemsa stain) of a patient with isolated congenital reduction of erythropoiesis in the bone marrow (pure red cell aplasia, PRCA). The haemoglobin concentration was 9.2 g/dL, white blood cell and platelet counts were normal.</p>
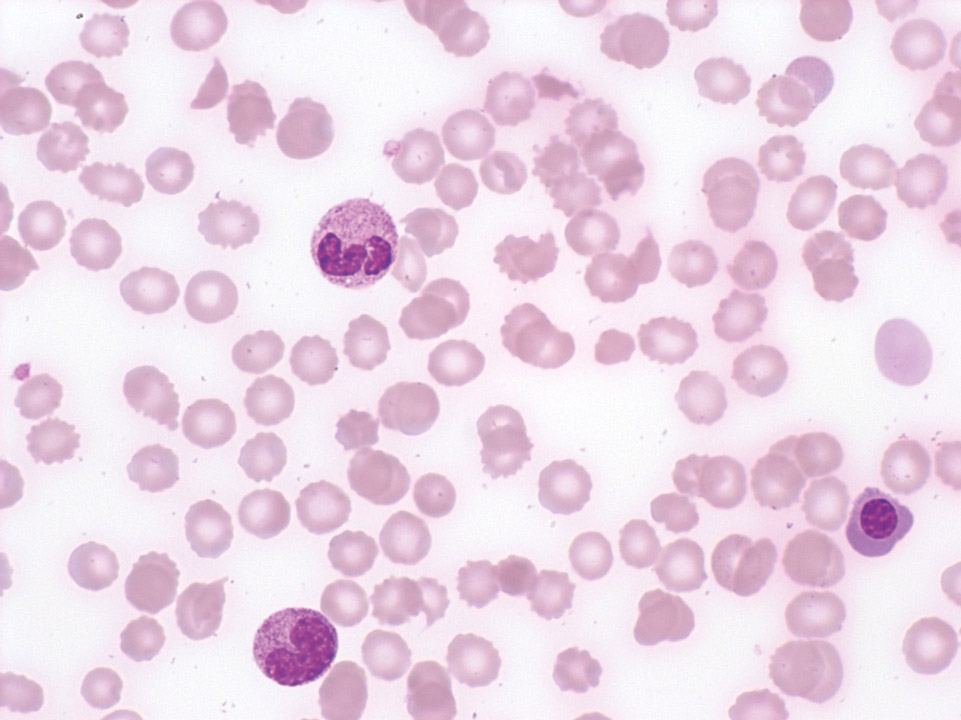
Leucoerythroblastic condition and schistocytes in a patient with colorectal carcinoma. The occurrence of schistocytes (->) in tumour patients is sometimes an indication of tumour infiltration of the bone marrow.
<p>Leucoerythroblastic condition and schistocytes in a patient with colorectal carcinoma. The occurrence of schistocytes (->) in tumour patients is sometimes an indication of tumour infiltration of the bone marrow.</p>
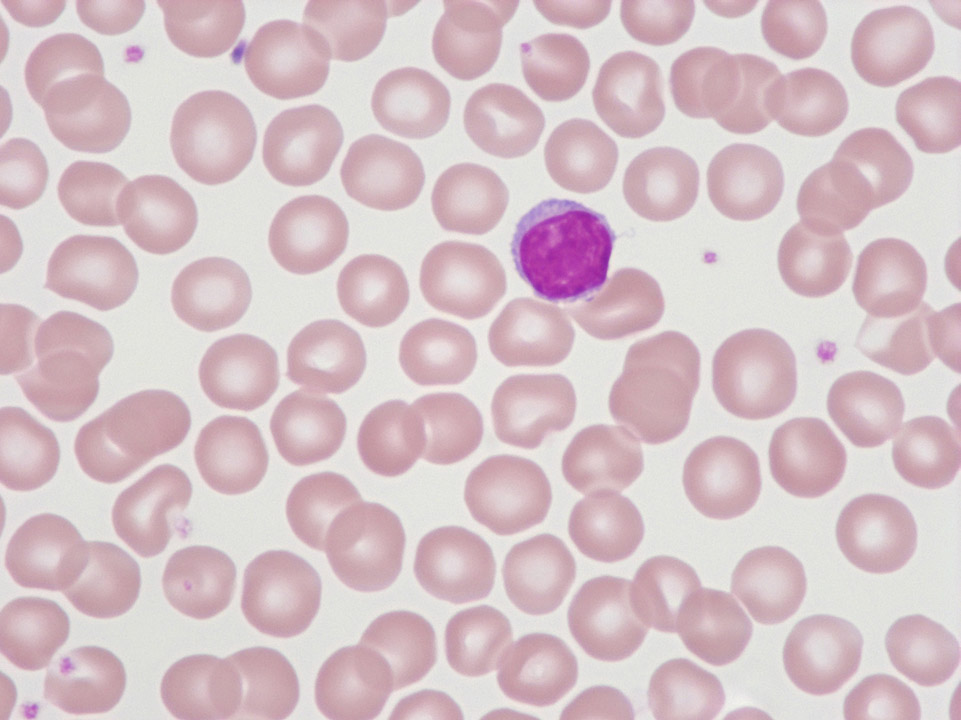
Cell description:
Size: 10-16 µm
Nucleus: round or slightly indented with condensed and cloddy chromatin, usually invisible nucleolus
Cytoplasm: scanty, weakly basophilic, may have small numbers of azurophilic granules
Morphologically functional subset of lymphocytes cannot clearly be distinguished.
Function: recognize and eliminate threats to the body. Lymphocytes of the innate immune system deliver an immediate response to viral attack. Lymphocytes of the adaptive immune system are specific to a particular antigen.
<p>Cell description: </p> <p>Size: 10-16 µm </p> <p>Nucleus: round or slightly indented with condensed and cloddy chromatin, usually invisible nucleolus </p> <p> Cytoplasm: scanty, weakly basophilic, may have small numbers of azurophilic granules </p> <p>Morphologically functional subset of lymphocytes cannot clearly be distinguished. </p> <p>Function: recognize and eliminate threats to the body. Lymphocytes of the innate immune system deliver an immediate response to viral attack. Lymphocytes of the adaptive immune system are specific to a particular antigen.</p>
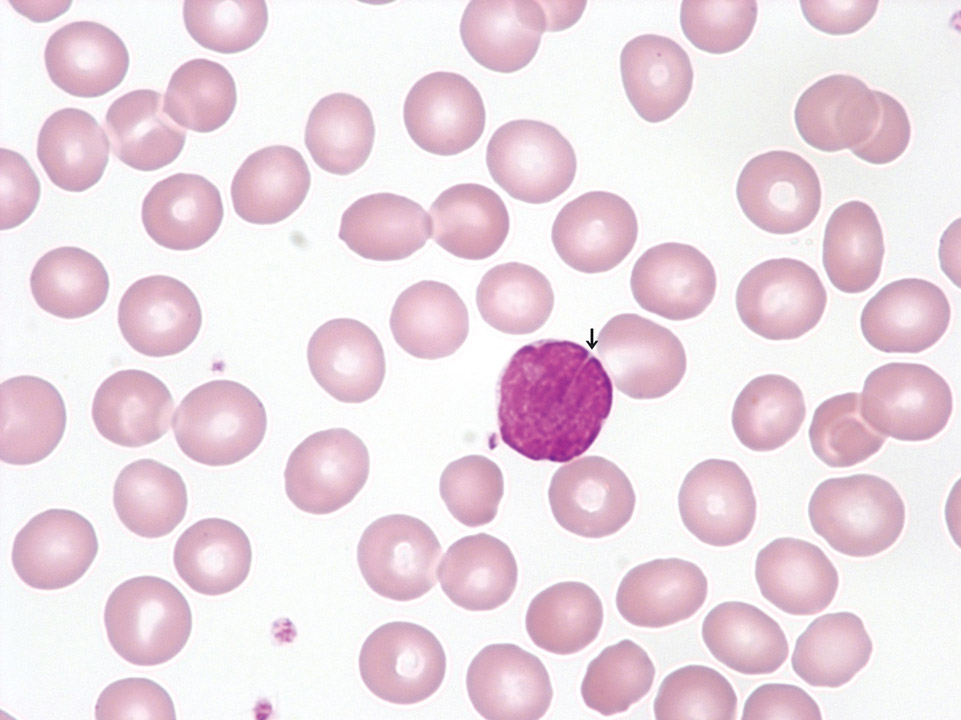
In the peripheral blood (May-Grünwald-Giemsa stain) of this patient lymphoma cells can be detected. They show a large, deeply indented nucleus (->) and scanty cytoplasm. Further diagnostics confirmed a mantle cell lymphoma.
<p>In the peripheral blood (May-Grünwald-Giemsa stain) of this patient lymphoma cells can be detected. They show a large, deeply indented nucleus (->) and scanty cytoplasm. Further diagnostics confirmed a mantle cell lymphoma.</p>
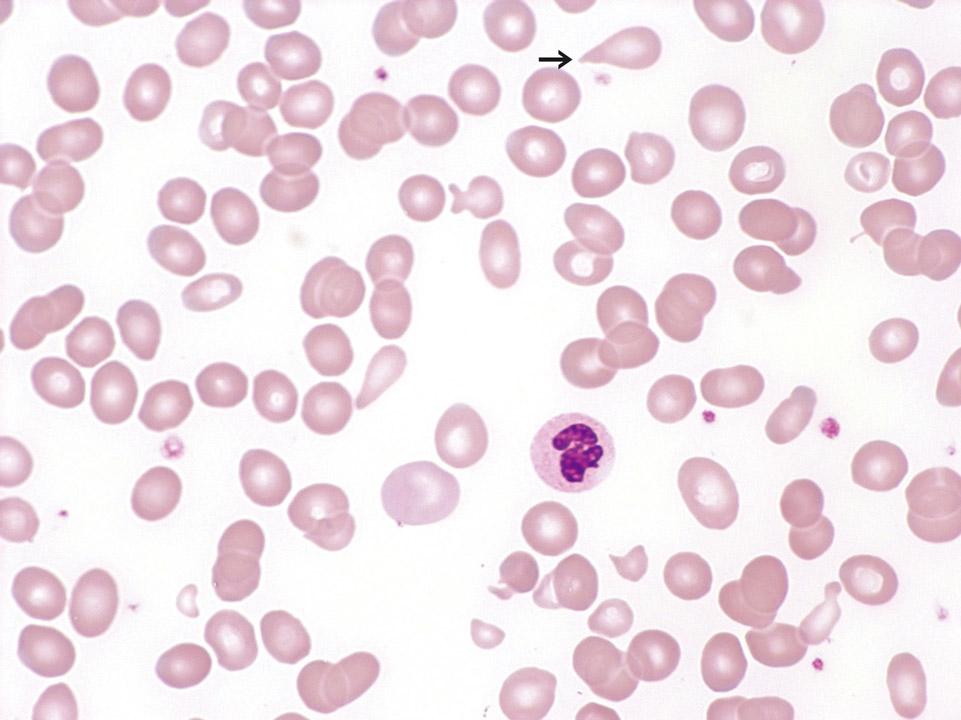
Peripheral blood (May-Grünwald-Giemsa stain) of an 82-year old patient with RCMD showing a macrocytic, hyporegenerative anaemia with clear changes of the red blood cells (micro- and macrocytosis, poikilocytosis and some teardrop cells (->)).
<p>Peripheral blood (May-Grünwald-Giemsa stain) of an 82-year old patient with RCMD showing a macrocytic, hyporegenerative anaemia with clear changes of the red blood cells (micro- and macrocytosis, poikilocytosis and some teardrop cells (->)).</p>